Portal:Medicine
The Medicine Portal

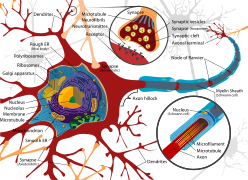
Medicine is the science and practice of caring for patients, managing the diagnosis, prognosis, prevention, treatment, palliation of their injury or disease, and promoting their health. Medicine encompasses a variety of health care practices evolved to maintain and restore health by the prevention and treatment of illness. Contemporary medicine applies biomedical sciences, biomedical research, genetics, and medical technology to diagnose, treat, and prevent injury and disease, typically through pharmaceuticals or surgery, but also through therapies as diverse as psychotherapy, external splints and traction, medical devices, biologics, and ionizing radiation, amongst others.
Medicine has been practiced since prehistoric times, and for most of this time it was an art (an area of creativity and skill), frequently having connections to the religious and philosophical beliefs of local culture. For example, a medicine man would apply herbs and say prayers for healing, or an ancient philosopher and physician would apply bloodletting according to the theories of humorism. In recent centuries, since the advent of modern science, most medicine has become a combination of art and science (both basic and applied, under the umbrella of medical science). For example, while stitching technique for sutures is an art learned through practice, knowledge of what happens at the cellular and molecular level in the tissues being stitched arises through science.
Prescientific forms of medicine, now known as traditional medicine or folk medicine, remain commonly used in the absence of scientific medicine and are thus called alternative medicine. Alternative treatments outside of scientific medicine with ethical, safety and efficacy concerns are termed quackery. (Full article...)
-
Debora Green (née Jones; born February 28, 1951) is an American physician who pleaded no contest to setting a 1995 fire that burned down her family's home and killed two of her children, and to poisoning her husband with ricin with the intention of causing his death. The case was sensational, and covered heavily by news media, especially in the Kansas–Missouri area, where the crimes occurred. Though Green has petitioned for a new trial twice in recent years, her requests have not been successful.
Green married Michael Farrar in 1979 while practicing as an emergency physician. The marriage was tumultuous, and Farrar filed for divorce in July 1995. Between August and September 1995, Farrar repeatedly fell violently ill, and despite numerous hospitalizations his doctors could not pinpoint the source of his illness. Green's emotional stability deteriorated and she began to drink heavily, even while supervising her children. On October 24, 1995, the Farrar family home, occupied by Green and the couple's three children — Timothy (age 13), Kate (age 10), and Kelly (age 6) — caught fire. Debora Green and Kate escaped without harm. Despite the efforts of firefighters, Timothy and Kelly died in the blaze. Investigation showed that trails of accelerant in the house led back to Green's bedroom, and that the source of Michael Farrar's intractable illness had been ricin, a poison served to him in his food by Green. (Full article...) -
Buruli ulcer (/bəˈruːli/) is an infectious disease characterized by the development of painless open wounds. The disease is limited to certain areas of the world, most cases occurring in Sub-Saharan Africa and Australia. The first sign of infection is a small painless nodule or area of swelling, typically on the arms or legs. The nodule grows larger over days to weeks, eventually forming an open ulcer. Deep ulcers can cause scarring of muscles and tendons, resulting in permanent disability.
Buruli ulcer is caused by skin infection with bacteria called Mycobacterium ulcerans. The mechanism by which M. ulcerans is transmitted from the environment to humans is not known, but may involve the bite of an aquatic insect or the infection of open wounds. Once in the skin, M. ulcerans grows and releases the toxin mycolactone, which blocks the normal function of cells, resulting in tissue death and immune suppression at the site of the ulcer. (Full article...) -
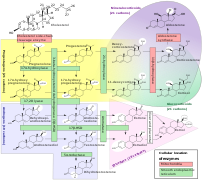
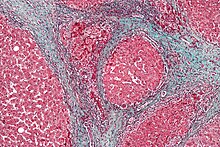
Endometrial cancer is a cancer that arises from the endometrium (the lining of the uterus or womb). It is the result of the abnormal growth of cells that have the ability to invade or spread to other parts of the body. The first sign is most often vaginal bleeding not associated with a menstrual period. Other symptoms include pain with urination, pain during sexual intercourse, or pelvic pain. Endometrial cancer occurs most commonly after menopause.
Approximately 40% of cases are related to obesity. Endometrial cancer is also associated with excessive estrogen exposure, high blood pressure and diabetes. Whereas taking estrogen alone increases the risk of endometrial cancer, taking both estrogen and a progestogen in combination, as in most birth control pills, decreases the risk. Between two and five percent of cases are related to genes inherited from the parents. Endometrial cancer is sometimes called "uterine cancer", although it is distinct from other forms of cancer of the uterus such as cervical cancer, uterine sarcoma, and trophoblastic disease. The most frequent type of endometrial cancer is endometrioid carcinoma, which accounts for more than 80% of cases. Endometrial cancer is commonly diagnosed by endometrial biopsy or by taking samples during a procedure known as dilation and curettage. A pap smear is not typically sufficient to show endometrial cancer. Regular screening in those at normal risk is not called for. (Full article...) -
Hepatorenal syndrome (often abbreviated HRS) is a life-threatening medical condition that consists of rapid deterioration in kidney function in individuals with cirrhosis or fulminant liver failure. HRS is usually fatal unless a liver transplant is performed, although various treatments, such as dialysis, can prevent advancement of the condition.
HRS can affect individuals with cirrhosis, severe alcoholic hepatitis, or liver failure, and usually occurs when liver function deteriorates rapidly because of a sudden insult such as an infection, bleeding in the gastrointestinal tract, or overuse of diuretic medications. HRS is a relatively common complication of cirrhosis, occurring in 18% of people within one year of their diagnosis, and in 39% within five years of their diagnosis. Deteriorating liver function is believed to cause changes in the circulation that supplies the intestines, altering blood flow and blood vessel tone in the kidneys. The kidney failure of HRS is a consequence of these changes in blood flow, rather than direct damage to the kidney. The diagnosis of hepatorenal syndrome is based on laboratory tests of individuals susceptible to the condition. Two forms of hepatorenal syndrome have been defined: Type 1 HRS entails a rapidly progressive decline in kidney function, while type 2 HRS is associated with ascites (fluid accumulation in the abdomen) that does not improve with standard diuretic medications. (Full article...) -
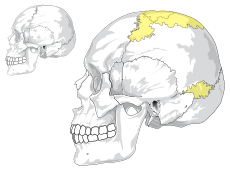
Meningitis is acute or chronic inflammation of the protective membranes covering the brain and spinal cord, collectively called the meninges. The most common symptoms are fever, intense headache, vomiting and neck stiffness and occasionally photophobia.
Other symptoms include confusion or altered consciousness, nausea, and an inability to tolerate light or loud noises. Young children often exhibit only nonspecific symptoms, such as irritability, drowsiness, or poor feeding. A non-blanching rash (a rash that does not fade when a glass is rolled over it) may also be present. (Full article...) -
Everywhere at the End of Time is the eleventh recording by the Caretaker, an alias of English electronic musician Leyland Kirby. Released between 2016 and 2019, its six studio albums use degrading loops of sampled ballroom music to portray the progression of Alzheimer's disease. Inspired by the success of An Empty Bliss Beyond This World (2011), Kirby produced Everywhere as his final major work under the alias. The albums were produced in Kraków and released over six-month periods to "give a sense of time passing", with abstract album covers by his friend Ivan Seal. The series drew comparisons to the works of composer William Basinski and electronic musician Burial, while the later stages were influenced by avant-gardist composer John Cage.
The series comprises six hours of music, portraying a range of emotions and characterised by noise throughout. Although the first three stages are similar to An Empty Bliss, the last three depart from Kirby's earlier ambient works. The albums reflect the patient's disorder and death, their feelings, and the phenomenon of terminal lucidity. To promote the series, anonymous visual artist Weirdcore created music videos for the first two stages. At first, concerned about whether the series would seem pretentious, Kirby thought of not creating Everywhere at all, and spent more time producing it than any of his other releases. The album covers received attention from a French art exhibition named after the Caretaker's Everywhere, an Empty Bliss (2019), a compilation of archived songs. (Full article...) -

Bupropion, formerly called amfebutamone, and sold under the brand name Wellbutrin among others, is an atypical antidepressant primarily used to treat major depressive disorder and to support smoking cessation. It is also popular as an add-on medication in the cases of "incomplete response" to the first-line selective serotonin reuptake inhibitor (SSRI) antidepressant. Bupropion has several features that distinguish it from other antidepressants: it does not usually cause sexual dysfunction, it is not associated with weight gain and sleepiness, and it is more effective than SSRIs at improving symptoms of hypersomnia and fatigue. Bupropion, particularly the immediate release formulation, carries a higher risk of seizure than many other antidepressants, hence caution is recommended in patients with a history of seizure disorder.
Common adverse effects of bupropion with the greatest difference from placebo are dry mouth, nausea, constipation, insomnia, anxiety, tremor, and excessive sweating. Raised blood pressure is notable. Rare but serious side effects include seizures, liver toxicity, psychosis, and risk of overdose. Bupropion use during pregnancy may be associated with increased odds of congenital heart defects. (Full article...) -
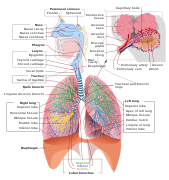
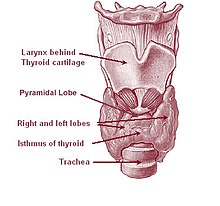
Thyrotoxic periodic paralysis (TPP) is a rare condition featuring attacks of muscle weakness in the presence of hyperthyroidism (overactivity of the thyroid gland). Hypokalemia (a decreased potassium level in the blood) is usually present during attacks. The condition may be life-threatening if weakness of the breathing muscles leads to respiratory failure, or if the low potassium levels lead to abnormal heart rhythms. If untreated, it is typically recurrent in nature.
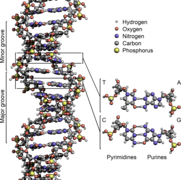
The condition has been linked with genetic mutations in genes that code for certain ion channels that transport electrolytes (sodium and potassium) across cell membranes. The main ones are the L-type calcium channel α1-subunit and potassium inward rectifier 2.6; it is therefore classified as a channelopathy. The abnormality in the channel is thought to lead to shifts of potassium into cells, under conditions of high thyroxine (thyroid hormone) levels, usually with an additional precipitant. (Full article...) -
Prostate cancer is the uncontrolled growth of cells in the prostate, a gland in the male reproductive system below the bladder. Early prostate cancer causes no symptoms. Abnormal growth of prostate tissue is usually detected through screening tests, typically blood tests that check for prostate-specific antigen (PSA) levels. Those with high levels of PSA in their blood are at increased risk for developing prostate cancer. Diagnosis requires a biopsy of the prostate. If cancer is present, the pathologist assigns a Gleason score, and a higher score represents a more dangerous tumor. Medical imaging is performed to look for cancer that has spread outside the prostate. Based on the Gleason score, PSA levels, and imaging results, a cancer case is assigned a stage 1 to 4. A higher stage signifies a more advanced, more dangerous disease.
Most prostate tumors remain small and cause no health problems. These are managed with active surveillance, monitoring the tumor with regular tests to ensure it has not grown. Tumors more likely to be dangerous can be destroyed with radiation therapy or surgically removed by radical prostatectomy. Those whose cancer spreads beyond the prostate are treated with hormone therapy which reduces levels of the androgens (male sex hormones) that prostate cells need to survive. Eventually cancer cells can grow resistant to this treatment. This most-advanced stage of the disease, called castration-resistant prostate cancer, is treated with continued hormone therapy alongside the chemotherapy drug docetaxel. Some tumors metastasize (spread) to other areas of the body, particularly the bones and lymph nodes. There, tumors cause severe bone pain, leg weakness or paralysis, and eventually death. (Full article...) -
Serpins are a superfamily of proteins with similar structures that were first identified for their protease inhibition activity and are found in all kingdoms of life. The acronym serpin was originally coined because the first serpins to be identified act on chymotrypsin-like serine proteases (serine protease inhibitors). They are notable for their unusual mechanism of action, in which they irreversibly inhibit their target protease by undergoing a large conformational change to disrupt the target's active site. This contrasts with the more common competitive mechanism for protease inhibitors that bind to and block access to the protease active site.
Protease inhibition by serpins controls an array of biological processes, including coagulation and inflammation, and consequently these proteins are the target of medical research. Their unique conformational change also makes them of interest to the structural biology and protein folding research communities. The conformational-change mechanism confers certain advantages, but it also has drawbacks: serpins are vulnerable to mutations that can result in serpinopathies such as protein misfolding and the formation of inactive long-chain polymers. Serpin polymerisation not only reduces the amount of active inhibitor, but also leads to accumulation of the polymers, causing cell death and organ failure. (Full article...) -
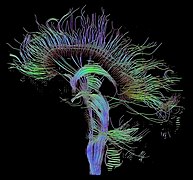
Schizophrenia is a mental disorder characterized by reoccurring episodes of psychosis that are correlated with a general misperception of reality. Other common signs include hallucinations (typically hearing voices), delusions (i.e., paranoia), disorganized thinking, social withdrawal, and flat affect. Symptoms develop gradually and typically begin during young adulthood and are never resolved. There is no objective diagnostic test; diagnosis is based on observed behavior, a psychiatric history that includes the person's reported experiences, and reports of others familiar with the person. For a diagnosis of schizophrenia, the described symptoms need to have been present for at least six months (according to the DSM-5) or one month (according to the ICD-11). Many people with schizophrenia have other mental disorders, especially substance use disorders, depressive disorders, anxiety disorders, and obsessive–compulsive disorder.
About 0.3% to 0.7% of people are diagnosed with schizophrenia during their lifetime. In 2017, there were an estimated 1.1 million new cases and in 2022 a total of 24 million cases globally. Males are more often affected and on average have an earlier onset than females. The causes of schizophrenia may include genetic and environmental factors. Genetic factors include a variety of common and rare genetic variants. Possible environmental factors include being raised in a city, childhood adversity, cannabis use during adolescence, infections, the age of a person's mother or father, and poor nutrition during pregnancy. (Full article...) -
Osteochondritis dissecans (OCD or OD) is a joint disorder primarily of the subchondral bone in which cracks form in the articular cartilage and the underlying subchondral bone. OCD usually causes pain during and after sports. In later stages of the disorder there will be swelling of the affected joint which catches and locks during movement. Physical examination in the early stages does only show pain as symptom, in later stages there could be an effusion, tenderness, and a crackling sound with joint movement.
OCD is caused by blood deprivation of the secondary physes around the bone core of the femoral condyle. This happens to the epiphyseal vessels under the influence of repetitive overloading of the joint during running and jumping sports. During growth such chondronecrotic areas grow into the subchondral bone. There it will show as bone defect area under articular cartilage. The bone will then possibly heal to the surrounding condylar bone in 50% of the cases. Or it will develop into a pseudarthrosis between condylar bone core and osteochondritis flake leaving the articular cartilage it supports prone to damage. The damage is executed by ongoing sport overload. The result is fragmentation (dissection) of both cartilage and bone, and the free movement of these bone and cartilage fragments within the joint space, causing pain, blockage and further damage. OCD has a typical anamnesis with pain during and after sports without any history of trauma. Some symptoms of late stages of osteochondritis dissecans are found with other diseases like rheumatoid disease of children and meniscal ruptures. The disease can be confirmed by X-rays, computed tomography (CT) or magnetic resonance imaging (MRI) scans. (Full article...) -
Subarachnoid hemorrhage (SAH) is bleeding into the subarachnoid space—the area between the arachnoid membrane and the pia mater surrounding the brain. Symptoms may include a severe headache of rapid onset, vomiting, decreased level of consciousness, fever, weakness, numbness, and sometimes seizures. Neck stiffness or neck pain are also relatively common. In about a quarter of people a small bleed with resolving symptoms occurs within a month of a larger bleed.
SAH may occur as a result of a head injury or spontaneously, usually from a ruptured cerebral aneurysm. Risk factors for spontaneous cases include high blood pressure, smoking, family history, alcoholism, and cocaine use. Generally, the diagnosis can be determined by a CT scan of the head if done within six hours of symptom onset. Occasionally, a lumbar puncture is also required. After confirmation further tests are usually performed to determine the underlying cause. (Full article...) -

Young people with polio receiving physiotherapy in the 1950s
The social history of viruses describes the influence of viruses and viral infections on human history. Epidemics caused by viruses began when human behaviour changed during the Neolithic period, around 12,000 years ago, when humans developed more densely populated agricultural communities. This allowed viruses to spread rapidly and subsequently to become endemic. Viruses of plants and livestock also increased, and as humans became dependent on agriculture and farming, diseases such as potyviruses of potatoes and rinderpest of cattle had devastating consequences.
Smallpox and measles viruses are among the oldest that infect humans. Having evolved from viruses that infected other animals, they first appeared in humans in Europe and North Africa thousands of years ago. The viruses were later carried to the New World by Europeans during the time of the Spanish Conquests, but the indigenous people had no natural resistance to the viruses and millions of them died during epidemics. Influenza pandemics have been recorded since 1580, and they have occurred with increasing frequency in subsequent centuries. The pandemic of 1918–19, in which 40–50 million died in less than a year, was one of the most devastating in history. (Full article...) -
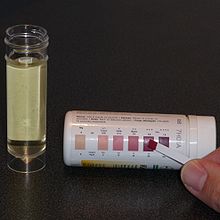
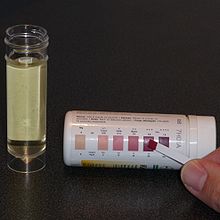
Testing for ketone bodies in urine
The ketogenic diet is a high-fat, adequate-protein, low-carbohydrate dietary therapy that in conventional medicine is used mainly to treat hard-to-control (refractory) epilepsy in children. The diet forces the body to burn fats rather than carbohydrates.
Normally, carbohydrates in food are converted into glucose, which is then transported around the body and is important in fueling brain function. However, if only a little carbohydrate remains in the diet, the liver converts fat into fatty acids and ketone bodies, the latter passing into the brain and replacing glucose as an energy source. An elevated level of ketone bodies in the blood (a state called ketosis) eventually lowers the frequency of epileptic seizures. Around half of children and young people with epilepsy who have tried some form of this diet saw the number of seizures drop by at least half, and the effect persists after discontinuing the diet. Some evidence shows that adults with epilepsy may benefit from the diet and that a less strict regimen, such as a modified Atkins diet, is similarly effective. Side effects may include constipation, high cholesterol, growth slowing, acidosis, and kidney stones. (Full article...)
Selected image –
WikiProject
Get involved by joining WikiProject Medicine. We discuss collaborations and all manner of issues on our talk page.
Related portals
-

Aniru Sahib Sahib Conteh (6 August 1942 – 4 April 2004) was a Sierra Leonean physician and expert on the clinical treatment of Lassa fever, a viral hemorrhagic fever endemic to West Africa caused by the Lassa virus. Conteh studied medicine at the University of Ibadan in Nigeria and taught at Ibadan Teaching Hospital. He later returned to Sierra Leone where he joined the Centers for Disease Control and Prevention (CDC) Lassa fever program at Nixon Methodist Hospital in Segbwema, first as superintendent and then as clinical director.
After the Sierra Leone Civil War began in 1991, the CDC closed their program in Segbwema. Conteh and his medical team moved from Segbwema to the Kenema Government Hospital (KGH), where he spent the next two decades running the only dedicated Lassa fever ward in the world. Conteh collaborated with the British charity Merlin to promote public health in Sierra Leone through education and awareness campaigns intended to prevent Lassa fever. With little funding and few supplies, Conteh successfully reduced mortality rates and saved many lives until an accidental needlestick injury led to his own death from the disease in 2004. (Full article...) -
Agent Orange is a chemical herbicide and defoliant, one of the tactical use Rainbow Herbicides.
It was used by the U.S. military as part of its herbicidal warfare program, Operation Ranch Hand, during the Vietnam War from 1961 to 1971. It is a mixture of equal parts of two herbicides, 2,4,5-T and 2,4-D. In addition to its damaging environmental effects, traces of dioxin (mainly TCDD, the most toxic of its type) found in the mixture have caused major health problems for many individuals who were exposed, and their children. (Full article...) -

The international pictogram for toxic chemicals.
The history of poison stretches from before 4500 BCE to the present day. Poisons have been used for many purposes across the span of human existence, most commonly as weapons, anti-venoms, and medicines. Poison has allowed much progress in branches, toxicology, and technology, among other sciences.
Poison was discovered in ancient times, and was used by ancient tribes and civilizations as a hunting tool to quicken and ensure the death of their prey or enemies. This use of poison grew more advanced, and many of these ancient peoples began forging weapons designed specifically for poison enhancement. Later in history, particularly at the time of the Roman Empire, one of the more prevalent uses was assassination. As early as 331 BCE, poisonings executed at the dinner table or in drinks were reported, and the practice became a common occurrence. The use of fatal substances was seen among every social class; the nobility would often use it to dispose of unwanted political or economic opponents. (Full article...) -
Aspirin (acetylsalicylic acid), an organic compound that does not occur in nature, was first synthesised in 1899.
In 1897, scientists at the drug and dye firm Bayer began investigating acetylated organic compounds as possible new medicines, following the success of acetanilide ten years earlier. Two years later, Bayer created acetylsalicylic acid, which they marketed around the world under the brand name "Aspirin". The drug was sold widely in the first half of the twentieth century, both by Bayer and by competing drug manufacturers. The name "aspirin" was so widely used that Bayer lost (or sold) the rights to the trademark in many countries. (Full article...) -
Obesity is a medical condition, sometimes considered a disease, in which excess body fat has accumulated to such an extent that it can potentially have negative effects on health. People are classified as obese when their body mass index (BMI)—a person's weight divided by the square of the person's height—is over 30 kg/m2; the range 25–30 kg/m2 is defined as overweight. Some East Asian countries use lower values to calculate obesity. Obesity is a major cause of disability and is correlated with various diseases and conditions, particularly cardiovascular diseases, type 2 diabetes, obstructive sleep apnea, certain types of cancer, and osteoarthritis.
Obesity has individual, socioeconomic, and environmental causes. Some known causes are diet, physical activity, automation, urbanization, genetic susceptibility, medications, mental disorders, economic policies, endocrine disorders, and exposure to endocrine-disrupting chemicals. (Full article...) -
John Benjamin Murphy, born John Murphy (December 21, 1857 – August 11, 1916) was an American physician and abdominal surgeon noted for advocating early surgical intervention in appendicitis appendectomy, and several eponyms: Murphy’s button, Murphy drip, Murphy’s punch, Murphy’s test, and Murphy-Lane bone skid. He is best remembered for the eponymous clinical sign that is used in evaluating patients with acute cholecystitis. His career spanned general surgery, orthopedics, neurosurgery, and cardiothoracic surgery, which helped him to gain international prominence in the surgical profession. Mayo Clinic co-founder William James Mayo called him "the surgical genius of our generation".
Over the course of his career he was renowned as a surgeon, a clinician, a teacher, an innovator, and an author. In addition to general surgical operations, such as appendectomy, cholecystostomy, bowel resection for intestinal obstruction, and mastectomy, he performed and described innovative procedures in neurosurgery, orthopedics, gynecology, urology, plastic surgery, thoracic surgery, and vascular surgery. He also ventured into techniques such as neurorrhaphy, arthroplasty, prostatectomy, nephrectomy, hysterectomy, bone grafting, and thoracoplasty. (Full article...) -
Pentasomy X, also known as 49,XXXXX, is a chromosomal disorder in which a female has five, rather than two, copies of the X chromosome. Pentasomy X is associated with short stature, intellectual disability, characteristic facial features, heart defects, skeletal anomalies, and pubertal and reproductive abnormalities. The condition is exceptionally rare, with an estimated prevalence between 1 in 85,000 and 1 in 250,000.
The condition has a large variety of symptoms, and it is difficult to paint a conclusive portrait of its phenotypes. Though significant disability is characteristic, there are so few diagnosed cases that confident conclusions about the presentation and prognosis remain impossible. Pentasomy X may be mistaken for more common chromosomal disorders, such as Down syndrome or Turner syndrome, before a conclusive diagnosis is reached. (Full article...) -
Trisomy X, also known as triple X syndrome and characterized by the karyotype 47,XXX, is a chromosome disorder in which a female has an extra copy of the X chromosome. It is relatively common and occurs in 1 in 1,000 females, but is rarely diagnosed; fewer than 10% of those with the condition know they have it.
Those who have symptoms can have learning disabilities, mild dysmorphic features such as hypertelorism (wide-spaced eyes) and clinodactyly (incurved little fingers), early menopause, and increased height. As the symptoms of trisomy X are often not serious enough to prompt a karyotype test, many cases of trisomy X are diagnosed before birth via prenatal screening tests such as amniocentesis. Research on females with the disorder finds that cases which were diagnosed postnatally, having been referred for testing because of obvious symptoms, are generally more severe than those diagnosed prenatally. Most females with trisomy X live normal lives, although their socioeconomic status is reduced compared to the general population. (Full article...) -
Shellfish allergy is among the most common food allergies. "Shellfish" is a colloquial and fisheries term for aquatic invertebrates used as food, including various species of molluscs such as clams, mussels, oysters and scallops, crustaceans such as shrimp, lobsters and crabs, and cephalopods such as squid and octopus. Shellfish allergy is an immune hypersensitivity to proteins found in shellfish. Symptoms can be either rapid or gradual in onset. The latter can take hours to days to appear. The former may include anaphylaxis, a potentially life-threatening condition which requires treatment with epinephrine. Other presentations may include atopic dermatitis or inflammation of the esophagus. Shellfish is one of the eight common food allergens, responsible for 90% of allergic reactions to foods: cow's milk, eggs, wheat, shellfish, peanuts, tree nuts, fish, and soy beans.
Unlike early childhood allergic reactions to milk and eggs, which often lessen as the children age, shellfish allergy tends to first appear in school-age children and older, and persist in adulthood. Strong predictors for adult-persistence are anaphylaxis, high shellfish-specific serum immunoglobulin E (IgE) and robust response to the skin prick test. Adult onset of fish allergy is common in workers in the shellfish catching and processing industry. (Full article...) -

Fig. 1. Pulvermacher's chain. The handles pointing away from the holder are insulated so that the physician can safely place the device in contact with any part of the patient's body.
The Pulvermacher chain, or in full as it was sold the Pulvermacher hydro-electric chain, was a type of voltaic battery sold in the second half of the 19th century for medical applications. Its chief market was amongst the numerous quack practitioners who were taking advantage of the popularity of the relatively new treatment of electrotherapy, or "electrification" as it was then known. Its unique selling point was its construction of numerous linked cells, rendering it mechanically flexible. A variant intended to be worn wrapped on parts of the body for long periods was known as Pulvermacher's galvanic chain or electric belt.
The Pulvermacher Company attracted a great deal of antagonism from the medical community due to their use of the names of well-known physicians in their advertising without permission. The nature of their business; in selling to charlatans and promoting quack practices also made them unpopular with the medical community. Despite this, the Pulvermacher chain was widely reported as a useful source of electricity for medical and scientific purposes, even amongst the most vocal critics of the Pulvermacher Company. (Full article...) -
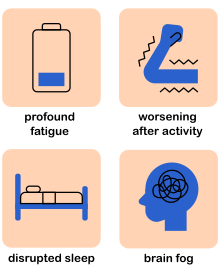
Myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) is a debilitating long-term medical condition. People with ME/CFS experience delayed worsening of the illness after minor physical or mental activity, which is the hallmark symptom of the illness. Other symptoms are a greatly reduced ability to do tasks that were previously easy, severe fatigue that does not improve much with rest, and sleep disturbances. Further common symptoms include dizziness or nausea when sitting or standing, along with memory and concentration issues and pain.
The cause or causes of the disease are unknown. ME/CFS often starts after a flu-like infection, for instance, after mononucleosis. In some people, physical trauma or psychological stress may also act as a trigger. ME/CFS can run in families, but the genes that contribute to ME/CFS risk are not known. ME/CFS is associated with changes in the nervous and immune systems, energy, and hormone production. Diagnosis is based on symptoms because no diagnostic test is available. (Full article...) -
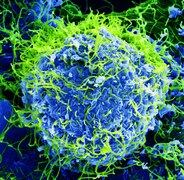
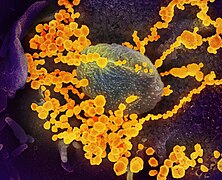
The human immunodeficiency viruses (HIV) are two species of Lentivirus (a subgroup of retrovirus) that infect humans. Over time, they cause acquired immunodeficiency syndrome (AIDS), a condition in which progressive failure of the immune system allows life-threatening opportunistic infections and cancers to thrive. Without treatment, the average survival time after infection with HIV is estimated to be 9 to 11 years, depending on the HIV subtype.
In most cases, HIV is a sexually transmitted infection and occurs by contact with or transfer of blood, pre-ejaculate, semen, and vaginal fluids. Non-sexual transmission can occur from an infected mother to her infant during pregnancy, during childbirth by exposure to her blood or vaginal fluid, and through breast milk. Within these bodily fluids, HIV is present as both free virus particles and virus within infected immune cells.
Research has shown (for both same-sex and opposite-sex couples) that HIV is untransmittable through condomless sexual intercourse if the HIV-positive partner has a consistently undetectable viral load. (Full article...) -
Iodine is a chemical element; it has symbol I and atomic number 53. The heaviest of the stable halogens, it exists at standard conditions as a semi-lustrous, non-metallic solid that melts to form a deep violet liquid at 114 °C (237 °F), and boils to a violet gas at 184 °C (363 °F). The element was discovered by the French chemist Bernard Courtois in 1811 and was named two years later by Joseph Louis Gay-Lussac, after the Ancient Greek Ιώδης, meaning 'violet'.
Iodine occurs in many oxidation states, including iodide (I−), iodate (IO−
3), and the various periodate anions. As the heaviest essential mineral nutrient, iodine is required for the synthesis of thyroid hormones. Iodine deficiency affects about two billion people and is the leading preventable cause of intellectual disabilities. (Full article...) -
Horace Gilbert Smithy Jr. (July 19, 1914 – October 28, 1948) was an American cardiac surgeon who in 1948 performed the first successful mitral valve repair (mitral valvulotomy) since the 1920s. Smithy's work was complicated because it predated heart-lung machines or open heart surgery. Though his procedure did not become a definitive treatment for valvular heart disease, he introduced the technique of injecting novocaine into the heart to avoid arrhythmias during surgery, and he showed that it was feasible to access and operate on the heart's valves.
A graduate of the University of Virginia School of Medicine, Smithy completed a surgical residency in Charleston, South Carolina, and then practiced surgery at Roper Hospital in Charleston. He also began working with a colleague in a dog laboratory to devise a valvulotomy (surgical treatment for diseased heart valves). Smithy's interest in heart valve dysfunction was also personal; he suffered from narrowing of the aortic valve related to rheumatic heart disease. (Full article...) -

Wasp stinger with a droplet of venom
Venom or zootoxin is a type of toxin produced by an animal that is actively delivered through a wound by means of a bite, sting, or similar action. The toxin is delivered through a specially evolved venom apparatus, such as fangs or a stinger, in a process called envenomation. Venom is often distinguished from poison, which is a toxin that is passively delivered by being ingested, inhaled, or absorbed through the skin, and toxungen, which is actively transferred to the external surface of another animal via a physical delivery mechanism.
Venom has evolved in terrestrial and marine environments and in a wide variety of animals: both predators and prey, and both vertebrates and invertebrates. Venoms kill through the action of at least four major classes of toxin, namely necrotoxins and cytotoxins, which kill cells; neurotoxins, which affect nervous systems; myotoxins, which damage muscles; and haemotoxins, which disrupt blood clotting. Venomous animals cause tens of thousands of human deaths per year. (Full article...)
Did you know –
- ...that the 47,XXY karyotype produces Klinefelter's syndrome, while 45,X causes Turner syndrome?
- ...that during the "Age of Heroic Medicine" (1780-1850), educated professional physicians aggressively practiced "heroic medicine", including bloodletting (venesection), intestinal purging (calomel), vomiting (tartar emetic), profuse sweating (diaphoretics) and blistering? These medical treatments were well-intentioned, and often well-accepted by the medical community, but were actually harmful to the patient.
- ...thalidomide is a drug that was sold during the late 1950s and 1960s to pregnant women as an antiemetic? It was later found to be teratogenic, causing amelia and phocomelia. However, it is still used for other indications such as for leprosy and multiple myeloma, with close regulation through the System for Thalidomide Education and Prescribing Safety (STEPS) program.
General images –
-
A cochlear implant is a common kind of neural prosthesis, a device replacing part of the human nervous system. (from History of medicine)
-
A 12th-century manuscript of the Hippocratic Oath in Greek, one of the most famous aspects of classical medicine that carried into later eras (from History of medicine)
-
"More Doctors Smoke Camels than Any Other Cigarette" advertisement for Camel cigarettes in the 1940s (from Medical ethics)
-
"Diagram of the causes of mortality in the army in the East" by Florence Nightingale. (from History of medicine)
-
Hippocrates (c. 460–370 BCE). Known as the "father of medicine". (from History of medicine)
-
The plinthios brochos as described by Greek physician Heraklas, a sling for binding a fractured jaw. These writings were preserved in one of Oribasius' collections. (from History of medicine)
-
A cuneiform terracotta tablet describing a medicinal recipe for poisoning (c. 18th century BCE). Discovered in Nippur, Iraq.
-
American combat surgery during the Pacific War, 1943 (from History of medicine)
-
Botánicas such as this one in Jamaica Plain, Boston, cater to the Latino community and sell folk medicine alongside statues of saints, candles decorated with prayers, lucky bamboo, and other items. (from Traditional medicine)
-
Magical stela or cippus of Horus inscribed with healing encantations (c. 332 to 280 BCE). (from History of medicine)
-
Galen (129–216 CE), known for his wide insights into anatomy. (from History of medicine)
-
Total healthcare cost per person. Public and private spending. US dollars PPP. For example: $6,319 for Canada in 2022. $12,555 for the US in 2022. (from Health care)
-
Medicine during the First World War - Medical Transport. (from History of medicine)
-
Life Expectancy of the total population at birth among several OECD member nations. Data source: OECD's iLibrary (from Health insurance)
-
Sometimes traditional medicines include parts of endangered species, such as the slow loris in Southeast Asia. (from Traditional medicine)
-
Guy's Hospital in 1820 (from History of medicine)
-
The numbers of Americans lacking health insurance and the uninsured rate from 1987 to 2008 (from Health insurance)
-
Life expectancy vs healthcare spending of rich OECD countries. US average of $10,447 in 2018. (from Health care)
-
A Neo-Assyrian cuneiform tablet fragment describing medical text (c. 9th to 7th century BCE). (from History of medicine)
-
Yarrow, a medicinal plant found in human-occupied caves in the Upper Palaeolithic period. (from History of medicine)
-
Jackson Memorial Hospital in Miami, the primary teaching hospital of the University of Miami's Leonard M. Miller School of Medicine and the largest hospital in the United States with 1,547 beds (from Health care)
-
Smallpox vaccination in Niger, 1969. A decade later, this was the first infectious disease to be eradicated. (from History of medicine)
-
Health Expenditure per capita (in PPP-adjusted US$) among several OECD member nations. Data source: OECD's iLibrary (from Health insurance)
-
Zhang Zhongjing - a Chinese pharmacologist, physician, inventor, and writer of the Eastern Han dynasty. (from History of medicine)
-
Health spending by country. Percent of GDP (Gross domestic product). For example: 11.2% for Canada in 2022. 16.6% for the United States in 2022. (from Health care)
-
Primary care may be provided in community health centers. (from Health care)
-
The Quaker-run York Retreat, founded in 1796, gained international prominence as a centre for moral treatment and a model of asylum reform following the publication of Samuel Tuke's Description of the Retreat (1813). (from History of medicine)
-
Seven named physicians and botanists of the Classical world from Vienna Dioscurides. Clockwise from top center: Galen, Dioscorides, Nicander, Rufus of Ephesus, Andreas of Carystus, Apollonius Mus or of Pergamon, Crateuas (from History of medicine)
-
Emil Kraepelin (1856–1926), the founder of modern scientific psychiatry, psychopharmacology and psychiatric genetics. (from History of medicine)
-
Statue of Robert Koch, father of medical bacteriology, at Robert-Koch-Platz (Robert Koch square) in Berlin (from History of medicine)
-
COVID-19 swab testing in Rwanda (2021). (from History of medicine)
-
Depiction of smallpox in Franciscan Bernardino de Sahagún's history of the conquest of Mexico, Book XII of the Florentine Codex, from the defeated Aztecs' point of view (from History of medicine)
-
National Hospital for Neurology and Neurosurgery in London, United Kingdom is a specialist neurological hospital. (from Health care)
-
Mexico City epidemic of 1737, with elites calling on the Virgin of Guadalupe (from History of medicine)
-
Global concentrations of health care resources, as depicted by the number of physicians per 10,000 individuals, by country. Data is sourced from a World Health Statistics 2010, a WHO report.[needs update] (from Health care)
-
A Ukrainian monument to the HIV pandemic. (from History of medicine)
-
Curandera performing a limpieza in Cuenca, Ecuador (from Traditional medicine)
-
Ethical prayer for medical wisdom by Dr Edmond Fernandes (from Medical ethics)
-
AMA Code of Medical Ethics (from Medical ethics)
-
Medical personnel place sterilized covers on the arms of the daVinci Xi surgical system, a minimally-invasive robotic surgery system, at the William Beaumont Army Medical Center. (from History of medicine)
-
A doctor checks a patient's pulse in Meiji-era Japan. (from History of medicine)
-
The emergency room is often a frontline venue for the delivery of primary medical care. (from Health care)
-
Mandrake (written 'ΜΑΝΔΡΑΓΟΡΑ' in Greek capitals). Naples Dioscurides, 7th century (from History of medicine)
-
Taoist symbol of Yin and Yang (from Medical ethics)
-
Patient, Surrey County Lunatic Asylum, c. 1850–58. The asylum population in England and Wales rose from 1,027 in 1827 to 74,004 in 1900. (from History of medicine)
-
healthcare expenditure in Japan by age group (from Health insurance)
-
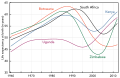
Most countries have seen a tremendous increase in life expectancy since 1945. However, in southern Africa, the HIV epidemic beginning around 1990 has eroded national health. (from History of medicine)
-
18th-century medical remedies collected by a British Gentry family (from History of medicine)
-
Sketch of Muslim physician Muhammad ibn Zakariya al-Razi (from History of medicine)
-
The Edwin Smith Surgical Papyrus, written in the 17th century BCE, contains the earliest recorded reference to the brain. New York Academy of Medicine. (from History of medicine)
-
Infographic showing how healthcare data flows within the billing process (from Medical billing)
More Did you know (auto generated)

- ... that the spotted lanternfly has been used in traditional Chinese medicine to treat swelling since the 1100s?
- ... that the Anglo-Saxons may have used a mixture of garlic, another Allium, wine, and bovine bile as an eye medicine?
- ... that Ala Stanford established the Black Doctors COVID-19 Consortium to fight racism in medicine, vaccinating nearly 4,000 people?
- ... that fourteenth-century Buddhist monk Tuệ Tĩnh is referred to as a founding father of traditional Vietnamese medicine?
- ... that Margaret C. Roberts was encouraged to study medicine by LDS Church leader Brigham Young to reduce mortality rates during childbirth?
- ... that Constance Fozzard was told during her surgical training that women with children could not become consultants?
Topics
Categories
Recognized content
Associated Wikimedia
The following Wikimedia Foundation sister projects provide more on this subject:
-
Commons
Free media repository -
Wikibooks
Free textbooks and manuals -
Wikidata
Free knowledge base -
Wikinews
Free-content news -
Wikiquote
Collection of quotations -
Wikisource
Free-content library -
Wikiversity
Free learning tools -
Wiktionary
Dictionary and thesaurus


























































![Image 38Global concentrations of health care resources, as depicted by the number of physicians per 10,000 individuals, by country. Data is sourced from a World Health Statistics 2010, a WHO report.[needs update] (from Health care)](http://upload.wikimedia.org/wikipedia/commons/thumb/1/1f/Global_physician_density_map_-_WHO_2010.png/120px-Global_physician_density_map_-_WHO_2010.png)